Summary:
Health
promotion covers all aspects of those activities that seek to improve the
health status of individuals and communities. Many studies have proved that
laughter has both, short term and long term benefits on our physical, mental
and emotional health. Our purpose was to assess role of Hasya Yog' in promotion
of health in the community. 400 people, of which 200 participated in Hasya Yog,
were assessed on the basis of three parameters; respiratory function assessed
by peak expiratory pressure and maximal inspiratory pressure, flexibility
measured by using a sit and reach test and quality of life was assessed by SF
36 questionnaire. Results were obtained using 'unpaired t test' and ‘Mann Whitney
Test’ for comparing the parameters. A significant difference was found while
comparing respiratory function using PEFR and PI max (p<0.001). Flexibility
test was also statistically significant (p < 0.01). In case of quality of
life physical health component was better in Hasya Yog members group whereas,
mental health component was not found to be statistically significant.
(p=0.24). Thus, Hasya Yog (Laughter clubs) definitely plays a major role in
promotion of health in the community, with respect to Respiratory function,
flexibility and quality of life (physical component). However, we found its limited
role in influencing the mental component of quality of life.
Hasya
Yog:
21st
of June 2015 is being celebrated as International Yog Day. The World
health organization (WHO) defines health as a state of complete physical,
mental and social wellbeing, and not merely an absence of disease or infirmity.
Health promotion is a part of primordial and primary approaches of health care
delivery system. It is the process of empowering people to make healthy
lifestyle choices and improve the quality of life. An article ‘Health Promotion
by Social Cognitive Means’ by Albert Bandura, examines health promotion and
disease prevention from the perspective of social cognitive theory. Active community
participation is crucial for any health promotion process to be successful.
India
is considered as the birth place of the Yog concept which has now got a global
recognition. Yog does not only help in developing the physical functioning and
health, but has also been proved to be extremely efficient in improvising the
mental and cognitive functions across all ages. In India, increase in self-help
clubs and voluntary organizations have also developed to encourage this. Janet Patford
and Helen Breen suggested that clubs attract older people by offering diverse
activities. Hasya Yog Mandal or “Laughter club” is one such social activity
started more than 13 years back. World Laughter Day was celebrated
recently on 3rd May. Joel Goodman said, “Seven days without laughter
makes one weak” and yes, laughing matters. An observational research done by
Colin Greaves proved that in 12 months, there were significant improvements in
depression and social support and marginally significant improvement in Short
Form 12 physical component in geriatric participants engaging in programs of
creative exercise and/or cultural activities with an emphasis on social interaction.
Tan SA, Tan LG et al proved that humour appears to attenuate
catecholamines and myocardial infarction (MI) recurrence and thus may be an
effective adjunct in post cardiac arrest care. Laughter has physiological, psychological,
social and spiritual benefits and also benefits in enhancing the quality of
life with hardly any adverse effects. Also practically there are no
contraindications of laughter. Therapeutic efficacy of laughter is mainly
derived from spontaneous laughter (triggered by external stimuli or positive
emotions) and self-induced laughter (triggered by oneself at will). However,
the medical literature contains little on humour, and very little research has
been conducted on this common aspect of human communication. Although
individual reviews and opinions are published regarding therapeutic use of
laughter an organized study on laughter is not reported. Our study assessed the
effect of these Hasya Yog mandals in promotion of health of the subjects by
indirectly assessing physical fitness components and quality of life in the
community dwelling elderly individuals.
We
performed a cross sectional survey in 2009-2010 in Pune city on 400 elderly
people of whom 200 subjects were regularly attending the laughter club
activities with at least 80% attendance while other 200 did not participate in
any other physical fitness activities except leisure walking and were selected
from the similar population as the Hasya Yog mandal members. Informed consent
was taken from all the subjects for their willingness to participate in the
survey which was approved by the local ethical committee. Outcome measures that
were used for assessing quality of life was the Short form 36 scale (SF36), for
assessing flexibility, the modified sit and reach test, for assessing
respiratory function the Peak Expiratory Flow Rate (PEFR) by Mini Wright’s peak
flow meter and maximum inspiratory pressure (PI max) by pressure gauge
instrument. These measurements were taken in a comfortably sitting position for
each subject and best of three readings was taken. Sit and reach test was
carried out for each subject after a prior warm up and mild stretching. Test was
done using a ruler and a marker as per feasibility. Any subject showing
symptoms of back pain while performing this test was excluded from the study. Quality
of Life (QoL) was measured by the SF-36 scale. The procedure of filling the
scale was explained and doubts, if any, were solved. However, this definitely
depended on the intelligence and understanding of the subjects which was not
under our control. Completed forms were collected from the members. Comparison
between two groups on the basis of respiratory function, flexibility and
quality of life was done using 'unpaired
t test' for comparing respiratory function
and flexibility parameters and ‘Mann Whitney Test’ for QoL with alpha set at p<0.05.
Table
1: Demographic Data:
|
Variable
|
Laughter
club group
|
Non
Laughter group
|
|
Samples
|
200
(Males
59, Females 121)
Excluded
20
|
200
(Males
52, Females 108)
Excluded
40
|
|
Age
(in yrs)
|
62.88
± 8.24 (Mean ± SD)
(n=180)
|
60.66
± 7.84 (Mean ± SD)
(n=160)
|
|
EXCLUDED
DATA SUBJECTS
|
Number
|
|
Smokers
|
08
|
|
Structural
Back Problems (Prolapsed Intervertebral Disc, Lysthesis etc.)
|
09
|
|
Obstructive
/ Restrictive Lung Pathology
|
06
|
|
Taking
Antidepressants / Anxiolytics
|
05
|
|
Additionally
Participating in Yoga / Health Clubs
|
14
|
|
Incomplete
filled Forms
|
05
|
|
Inability
To Perform Tests
|
13
|
|
TOTAL
|
60
|
Table
2: Comparison between both the groups on the basis of respiratory function, flexibility
and quality of life.
|
Variable
|
Laughter
club group (mean ± SD)
|
Non
Laughter group (Mean ± SD)
|
p
Value
|
|
PEFR
(Lt/ min)
|
278.58
± 75.5
|
239
± 78
|
<
0.05
|
|
Pi
Max (cms H2O)
|
75.21
± 44.58
|
57.3
± 32.9
|
<
0.05
|
|
Flexibility
(cms)
|
30.4
± 9.375
|
27.74
± 9.733
|
=
0.01
|
|
Physical Function
|
87.5
± 13.8
|
79.84
± 19.95
|
<
0.05
|
|
Role Physical
|
83.34
± 19.37
|
79.76
± 21.8
|
<
0.05
|
|
Bodily Pain
|
79.08
± 19.91
|
66.24
± 24.54
|
<
0.05
|
|
General Health Perceptions
|
75.77
± 18.09
|
68.03
± 27.85
|
<
0.05
|
|
Role Emotional
|
84.82
± 21.6498
|
78.2
± 21.75
|
=
0.24
|
|
Vitality
|
81.61
± 19.58
|
68.75
± 25.25
|
=
0.24
|
|
Mental Health
|
83.06
± 15.6
|
77.15
± 22.53
|
=
0.24
|
|
Social Function
|
96.1
± 10.25
|
95.51
± 9.0361
|
=
0.24
|
|
Physical
Component
Summary
|
81.43
± 11.79
|
73.46
± 14.85
|
<
0.05
|
|
Mental
Component Summary
|
86.4274
± 11.4413
|
79.903
± 12.50
|
=
0.24
|
The
values obtained and analysed showed a significant difference (p<0.001)
between peak expiratory flow rate, maximal inspiratory pressure, flexibility by
sit-and-reach test, physical QoL and physical QoL components between both the group.
Difference between scores of mental QoL and mental QoL components scale were
not found to be significant (p>0.001).
How
Does Laughter (Hasya Yog) Help Us?
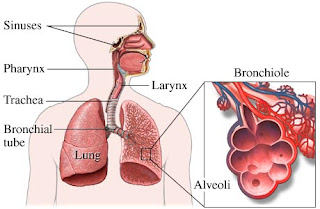
Impact
of laughter on general well-being of patients is been described, however an
organized controlled study in laughter clubs is not been done. The function of respiratory
system depends on many factors out of which important ones are the central
nervous system with the neural pathways and the muscles of respiration and
chest wall. The lungs are not capable of inflating themselves. The force for this
inflation must be supplied by the muscles of respiration. Respiratory function
was taken as a surrogate measure for physical functions. It was judged by two
parameters: PEFR and PI max. These are the indicators of expiratory and
inspiratory function respectively. Hasya Yog members demonstrated a significant
difference in both. Hence, their respiratory function was better than the non-participants
in laughter group. However, low PEFR and PI max scores might also be due to the
subclinical conditions which were not assessed by us. The above obtained result
is supported by research findings which proved that respiratory system is
coordinated in a rather precise way with laryngeal activity during a laugh.
Phasic respiratory efforts are present during laughter. Laughter involves deep
inspiration followed by forceful exhalation. Due to increased respiratory
muscle strength by regular laughter therapy, indirectly we must have got good
scores of PEFR and PI max. Flexibility training is an integral part of the laughter
club protocol wherein stretching exercises are been given to all the members of
laughing for initial 10 minutes.
Muscles
shorten and lose elasticity, due to increased cross linking between collagen
tissues that occurs with normal aging process. In our study flexibility of hamstrings
and back was assessed by sit and reach test and was found to be good in Hasya
Yog members. This improved flexibility may in turn reduce the chances of having
any further musculoskeletal ailments, pains, gait limitation and risks of
falling. This was reflected in our study by better physical quality of life
score in this group. Cunha et al too found that stretching exercises were
effective in reducing pain and improving range of motion and quality of life in
female patients with chronic neck pain. Stretching adds to functional fitness,
helping to stay agile and independent as long as possible, improving general health.
Static stretching is preferred to create long lasting lengthening of muscles
and surrounding tissue. It is a safe and well tolerated form of stretching. This
might be the reason why static stretching techniques practiced in laughter
clubs were beneficial.
Physical
activity improves patients’ ability to perform tasks and patient’s perception
of impact of disability on their physical functioning. There was significant
difference in the physical component summery (PCS) scores between Hasya Yog group
and other group. PCS includes four components physical functioning (PF), role
limitation due to physical health problems (RP), bodily pain (BP) and general
health perception (GP). Hasya Yog group showed higher mean scores for all and reported
less limitation in doing activities of daily living (ADLs) like carrying
household stuff, stair climbing, walking etc. All exercises of laughter club help
in performing activities more efficiently. Whereas; people in non-laughter
group and having sedentary life style leads to reduction in their physical
abilities due to disuse. In the laughter group, we got significantly low score
for pain. This is supported by the research which showed that laughter and
distraction both increased the pain tolerance by causing release of endorphins
which are natural pain suppressors. Their general health perception reported was
also good. This is supported by research article published in American medical association’s
journal, which conclude that “A humour therapy program can increase the quality
of life for patients with chronic problems and that laughter has an immediate
symptom-relieving effect for these patients, an effect that is potentiated when
laughter is induced regularly over a period.” Series of researches did by Dr.
Lee Berk and colleague put forth the fact that laughter therapy increases level
of activated T cell, antibodies IgA, gamma interferon, IgB which ultimately
increases the immunity. A lot of interaction between peers facing similar
problems might help them to cope with the diseases better and increase the
self-confidence. This might be reflected in the results as, experimental group
showed positive perception about their health.
Mean
score for quality of life (mental component) in the laughter group was higher
as compared to the other group. However, statistical comparision did not show a
significant difference as p = 0.24. Mental component summary is calculated
using four components of SF-36 scale; role limitation due to emotional health
problems (RE), mental health (MH), vitality (VT) and social functioning (SF).
Laughter club members showed higher scores on first three parameters. Scores
for social functioning was found to be similar for both the groups. It is also
subjective and equally dependent upon the interpretations and perceptions of
the individual. This could be the reason why laughter club activities might not
be having a significant role in influencing mental health of an individual.
Research indicates that interventions, which promote active social contact,
which encourage creativity, and which use mentoring, are more likely to
positively affect health and well-being. Clubs provide a forum where people can
meet, talk, and receive social acknowledgement on a regular basis. They thus
help to foster a sense of connectedness and may reduce the loneliness that
older people often experience as a result of retirement, bereavement, and children
moving away. Laughter works as a safety valve that diffuses tension, reduces
stress related hormones like epinephrine, cortisol etc. and aids in relaxation.
In our study, the Hasya Yog group showed a positive response to questions about
feeling calm and peaceful which is also supported by a recent study indicating that
laughter resulted in H-reflex suppression. Both laughter and simulated laughter
decreased spinal motor excitability causing muscle relaxation and reducing
stress. People who are engaged in any of the social activities get an
opportunity to share their emotions, might feel the intensity of such problems less
as compared to others who are socially isolated. Thus, summing all the
researches and results observed in our study, we can conclude that
participation in a regular exercise program and engaging in social activities
as in laughter clubs is an effective intervention.
Thus,
we concluded that Hasya Yog (Laughter therapy) definitely play a major role in promotion
of health in community with respect to respiratory function, flexibility and
quality of life (physical component). However, its role was found to be limited
in influencing the mental component of quality of life.
We
would like to thank all the participants who participated in the study with
co-operation and enthusiasm.
Dr.
Nishigandha R Supekar (PT)
Dr.
Apurv P Shimpi (PT)
Dr.
Alopa V Madane (PT)
The above study has been published in
the Indian Journal of Physiotherapy & Occupational Therapy, April-June
2014, Vol. 8, Issue. 2; Page 110-114